THE HUMANA STORY
ENHANCING EXPERIENCES WITH VEDA’S AUTOMATION TECHNOLOGY
While Humana historically was making millions of calls annually to confirm provider data, ongoing inconsistencies and inaccuracies in these directories can make it harder to find a provider and lead to administrative burden for seniors, providers, and health plans.
Learn how Humana's partnership with Veda helps seniors get real-time access to local in-network providers
VECTYR CURATED DATASET
Data Curation
The most up-to-date, comprehensive, and accurate source of data on healthcare providers, groups, and facilities on the market. Curated with data from over 100,000 unique sources, your organization can access accurate profiles of over 3.5 million active providers.
HOW IT WORKS
Velocity Process Automation
Speed & Data Quality
It’s as easy as clicking “upload.” Once your roster enters the Veda platform, Velocity formats, verifies and updates your files in under 24 hours, delivering a clean version that is structured for your industry and preferred output. Our AI-driven automation reduces the manual load on your team, freeing them up for more value-based efforts.
HOW IT WORKS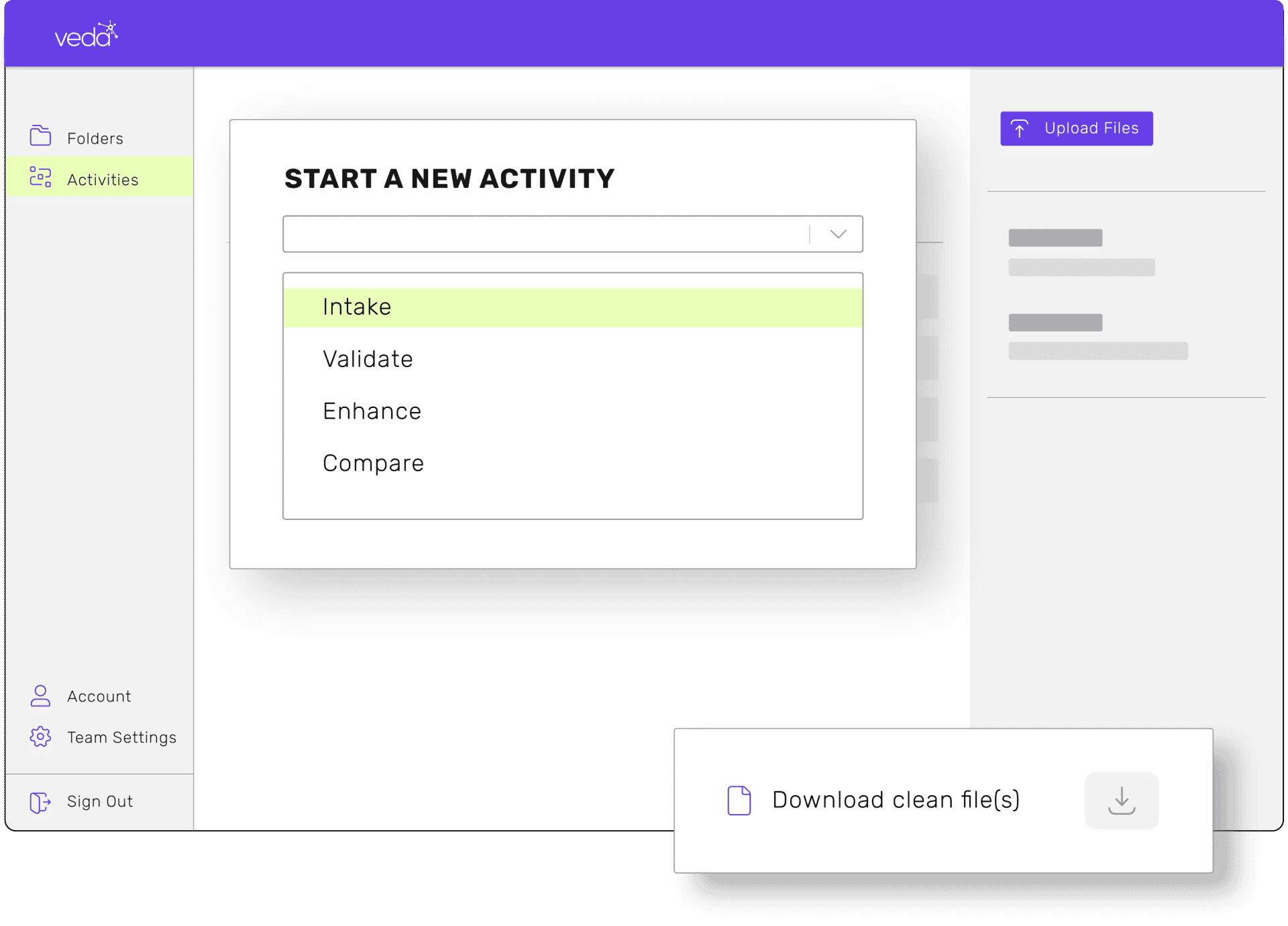
QUANTYM DATA QUALITY SCORING
ACCURACY & SCORING
When it’s time to give your database the ultimate deep clean, let Veda do the dirty work. Quantym performs a detox of your entire provider directory and analyzes your data for accuracy, quality, and thoroughness. It reconciles and validates your existing content, while reworking your bad data, then provides the correct course of action to make further data improvements.
HOW IT WORKS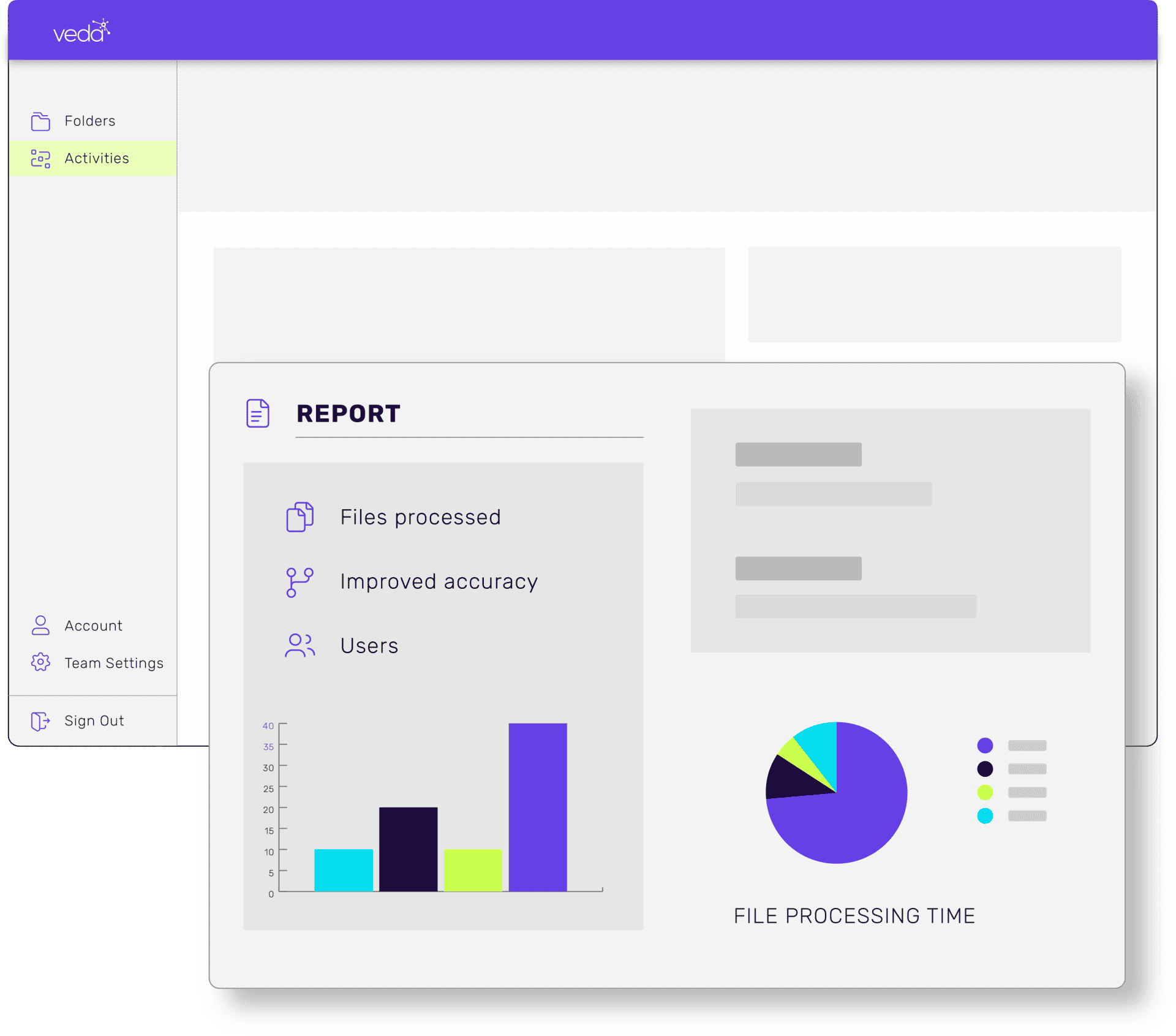
Use Cases & Resources
VIEW ALLTHE TOP CHOICE FOR HEALTH CARE
We’re the authority on health plan data. See how Veda’s Smart Automation platform can work for your health plan. Improve data accuracy, reduce workloads, and enhance the member experience. But first, start with a free data assessment.

No comments found