As a part of our interview series called “5 Things I Wish Someone Told Me Before I Became A Founder”, I had the pleasure of interviewing Meghan Gaffney.
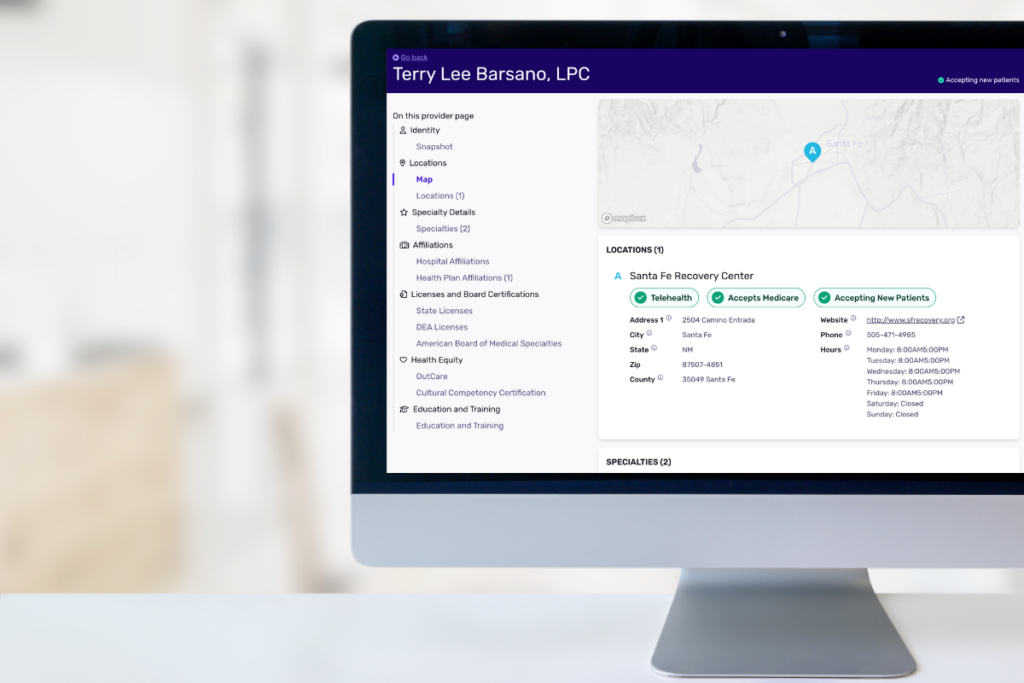
Meghan Gaffney is Co-Founder and CEO of Veda, a company that blends science and imagination to solve healthcare’s most complex data issues with human-in-the-loop Smart Automation. Meghan has over 15 years of experience working with elected officials and impact organizations, as well as consulting on technology opportunities. She is a passionate advocate for artificial intelligence and machine learning and believes these technologies will create unprecedented economic opportunities for the United States and the world.
Thank you so much for joining us in this interview series! Can you tell us a story about what brought you to this specific career path?
I stumbled into this career after having built a first career for myself in politics and policy. I worked in D.C. around the time the Affordable Care Act was being legislated, and that was actually what inspired me to focus specifically on healthcare. I kept hearing about all the administrative waste in the industry and the lack of solutions to address it–and I knew this was going to become my mission.
Can you tell us a story about the hard times that you faced when you first started your journey?
When I was working to take Veda from an idea to a reality, it was one of the most challenging periods of my life. As a woman in a male-dominated space, who had never worked directly in the actual industry I was trying to disrupt, it took a long time to feel the confidence I projected outwardly during all those early business pitches.
I immediately felt a sense of imposter syndrome when Veda landed its first customer, and I began our investor search.
Where did you get the drive to continue even though things were so hard?
When I was navigating the healthcare industry as a single mom, I was frustrated by the amount of time I put into things I felt should be simple–like finding an in-network doctor for my son. Not to mention how much time I spent in waiting rooms filling out paperwork instead of being with my kids. I took that frustration and turned it into a conviction to develop technology that could give people back their time and allow them to turn their attention to the things they care about. That applies as much to mothers and fathers as it does to providers and insurers.
So, how are things going today? How did grit and resilience lead to your eventual success?
Things are going exceedingly well. It’s been an exciting time, particularly since the pandemic, which accelerated our business but, of course, took a lot of grit and resilience. One step I took was focusing on building a strong executive team. This allowed me to have my role shift from exclusively driving to also listening, learning, and taking in the skills and lessons that my executive team has to offer. I’m always learning, and it makes my job exciting because I’m seeing how to elevate the company by listening to people who have done this before. Grit doesn’t just have to come from within–I’ve learned it’s ok, it’s actually beneficial, to lean on others.
Can you share a story about the funniest mistake you made when you were first starting? Can you tell us what lesson you learned from that?
If I think back to the early days, there are many I could mention. One that will always stand out came about when we were ready to sign one of our first big potential contracts with a large national health plan. We were excited about finalizing the contract, but we quickly realized that our business couldn’t operate out of my co-founder’s basement! We needed an actual business address to execute this contract and everyone after that. There were so many logistical things we hadn’t dealt with yet because our business was growing so quickly. Of course, with this contract, we quickly secured office space and a secure network, and that really elevated our team’s morale, in addition to the practical aspects!
What do you think makes your company stand out? Can you share a story?
One of the things that has remained consistent within our company from the very first day until today is that while we have a very technical product, when it comes to our culture, we have kept the focus on our people. One of the first examples I think of is earlier on, during the COVID-19 pandemic, I realized that we wouldn’t be seeing our colleagues in the office any time soon. So, I drove to every one of our employees’ houses and took a walk with them, just to check in with everyone and ensure we continued to build our relationships. Whether it’s virtual or in-person lunches with teams across the company or going for a walk, we are still doing that today and I believe it’s key to making our business thrive.
Which tips would you recommend to your colleagues in your industry to help them to thrive and not “burn out”?
The biggest piece that has been so helpful for me is building a team that is full of smart, hardworking, and trustworthy people. When you have a great team, you’re able to take a step back when you need to. It’s so reassuring to know that when you take a vacation, you have a team you fully trust, and that business will continue as usual. In fact, I think the test for any new founder is if they able to take a vacation. That’s how you know you’re doing things right!
None of us are able to achieve success without some help along the way. Is there a particular person who you are grateful towards who helped get you to where you are? Can you share a story?
I will always be so grateful to my co-founder and partner, Dr. Bob Lindner. We met in 2015 through a mutual friend and connected over our shared vision of creating real impact for people. He was an astrophysicist who agreed to come along on this wild ride of transforming healthcare with me, and he’s supported me in my founder’s journey from the beginning. After a pitch presentation that truly knocked down my confidence, Bob took me aside and said to me, “I see you.” He meant that he could see how much of myself I’d poured into Veda and how hard I’d worked. “I see you” became a mantra for me, that reminded me that I was enough, and I could build this company, whenever I started to falter.
How have you used your success to bring goodness to the world?
Most of the technological solutions being built today in healthcare are focused on improving the patient experience — which is a dire need. But the industry can’t fully deliver on the promise of patient-centered care until all the problems and inefficiencies within its infrastructure are addressed, like its estimated $1 trillion in administrative spend. In 2021, we saved health plans thousands of hours of processing time and countless dollars, and those insurers gained time and resources to focus where they are passionate — keeping members healthy.

What are your “5 things I wish someone told me before I started leading my company” and why. Please share a story or example for each.
- Be Ready For Your Moment to Accelerate. For many of you, at some point in your journey, outside forces in the universe will align to create an opportunity for accelerated growth. When that happens, you need to be open and ready to take on these new challenges and see the opening for your business. For example, during the pandemic, my company had to evolve our business strategy, and make much more solid cases to our potential customers, not to mention our investors. But as a result of our hard work, and our laser focus on solving our customers’ problems, which changed a bit due to this global crisis, we were very successful. And we felt good about it, because we were able to help keep the healthcare system going at a critical time.
- Every “no” gets you closer to a “yes”. I got this advice from my dad, who taught us as kids to always get up and keep going after getting knocked down. I’ve needed to remind myself to keep going even as people challenged me with questions like “. Can I run this company while also raising young kids?” That’s an actual question asked of me by an investor! To me, I took this as a sign that those weren’t the people who were the right partners for me. And that’s just one example of many “punches” I took on this founder path. But I was patient, and when the right people came along that truly saw our vision and wanted to see me and our company succeed, I welcomed them with open arms.
- Integrate points of view and expertise from outside your industry. Me and many of my colleagues at Veda come from non-traditional, non-healthcare backgrounds. While we may not have all taken the traditional industry path, when we combine our areas of expertise, we see that we’re actually able to make a huge positive impact on people’s health. We were able to look at problems many had deemed unsolvable and find solutions, because we brought scientific, policy, and a host of other areas of expertise. And then, of course, we also made sure we studied the healthcare industry and that we made strategic hires with deep expertise in health.
- Building the right C-suite and full team will take time–but it’s worth the wait. There’s no rulebook for how to build your C-suite, your larger team, and your company culture. My advice is to hire people who will challenge you, push your boundaries on innovation, and share different perspectives, particularly in your C-suite. Once you have the right team backing you, your business will truly take off. As an example, our Chief People Officer actually comes from the hospitality industry, and I knew when we met her that she had that inquisitive mind that we value at Veda. Her dominating skill was challenging people to reach to achieve and build a business to accelerate their success. She challenges me and offers different viewpoints and makes sure that ALL of our people are fulfilled.
- It’s never too early to protect any IP your company creates. We started filing for patents right away at my company–our initial investors actually thought we were nuts! But I argue that this is a strategy every tech company should follow. Why? Because it takes a really long time to go through the process–from application to securing patents, we were looking at years, not months or weeks. It’s really important when you’re fully confident in what you have built, that you start ensuring it’s protected. That’s not just important for you–it’s crucial for your customers. A strong IP portfolio is an outstanding competitive differentiator, certainly in health tech and absolutely in the broader tech industry as well.
Can you share a few ideas or stories from your experience about how to successfully ride the emotional highs & lows of being a founder”?
It’s amazing to be a woman representing other women in health tech, but it’s not always easy, especially when running your own company. I’ve found the highs are just as impactful as the lows and I’ve carried resilience and confidence with me through my entire founder’s journey. I love mentoring and speaking to other women about how to have confidence and pursue their dreams. I know I’m privileged in my position, and I do my best to share lessons learned and kick a hole through every glass ceiling.
You are a person of great influence. If you could start a movement that would bring the most amount of good to the most amount of people, what would that be? You never know what your idea can trigger. 🙂
I spend a lot of time thinking about how to create a technology community? that reflects the communities we serve. Oftentimes, the people who have the greatest experience with the healthcare challenges that technology should be solving face barriers from becoming the innovators to address them.
How can our readers further follow your work online?
This was very inspiring. Thank you so much for joining us!