Medica’s Director of Provider Network Operations & Initiatives, Patty Franco, sat down with Veda to talk about all things provider data and directories. As a current Veda client, Medica is making targeted changes to their directory resulting in improved accuracy and positive member experience.
Tell us about Medica, what areas does your health plan cover?
Our nonprofit health plan serves about 1.5 million members in 12 states: Minnesota, Arizona, Illinois, Iowa, Kansas, Missouri, Nebraska, North Dakota, Oklahoma, South Dakota, Wisconsin, and Wyoming. I’ve been with Medica for over 18 years.
I’ve been with Medica for over 18 years and we’ve had some exciting changes recently, such as our merger with Dean Health Plan out of Madison, Wis. Our plans combined have a better opportunity to support the healthcare needs of members and to further enhance our provider relationships.
From a provider data collection, ingestion, and validation standpoint, what was Medica’s process before partnering with Veda?
Medica receives data from providers in a number of ways: our portal, delegated rosters, forms, new contracts, and more. Depending on how that data comes in, it will be processed by our teams to get provider demographics and reimbursement set up in our systems.
As to what we were doing to ensure accuracy, that too had many options — none of them ideal. We used manual audits throughout the processing of the data and also performed a monthly audit of all our directory (public-facing) data. This audit is what is used to determine where we have inaccuracies. The audit includes randomly selected records in which we make secret shopper calls and ask the same questions CMS does in their audit.
Can you explain your data lifecycle?
Our process with Veda is to use a monthly file that we give to Veda and Veda runs through their Smart Automation tools and provides a response back in two days. We use the responses and run them through a series of queries that sorts the data we want to address and correct. Depending on the edit, it may be automated into our system and corrected. If needed, it could be something we want to do further investigation on so we will send that to another team to do that research, such as validation with a practitioner.
Veda’s tools get us started in the right direction and, more often than not, we can put their suggested correction directly into our system.
All health plans have different internal structures. What teams in your organization interact with provider and practitioner data?
So many departments within Medica interact with our provider data. Network Management, Provider Finance, Provider Operations, Provider Call Center, Reporting & Analytics, and Health Services all use it.
What have you found to be an industry best practice in terms of using Veda to maintain high data accuracy?
Veda supplements the various sources we receive data from and validates the accuracy of it. Plus, Veda has helped us use claims data to obtain information for providers that do not submit any claims or have limited claims.
Of course, we still use some internal tools, but Veda has helped us pinpoint areas we can focus our attention on with relative ease. For example, we’ve been able to better work with our contract managers to address gaps in provider data. We’ve also learned to reframe our contract language for delegated agreements to ensure that providers maintain their data with us.
What challenges and opportunities did you encounter, internally and externally, on your path to success?
Internally, when you add a new vendor or service, it is all about the training and handoffs to other departments and systems. How many systems you have that hold this data can be challenging along with ever-changing technology. Processes that have to remain manual are a challenge, but necessary. And of course, executive buy-in and understanding took time, as did budget approval.
Externally, we are still working on drilling down using data-cleansing processes with our delegates. They account for about 50% of our data, so they are important partners in getting the data accurate on the way in. As we know, the root of bad data starts at ingestion. With targeted recommendations from Veda, we identified where the worst data issues were coming from. This allowed us to rethink how we interact with the data on the front end. Now, if we see a roster with 30 locations for one provider, we call and inquire about it.
It is imperative to both our organizations to have accurate data so that our members can find providers in our directories and that the phone number is correct so they get an appointment quickly to address their health care needs.
How do you approach making changes internally?
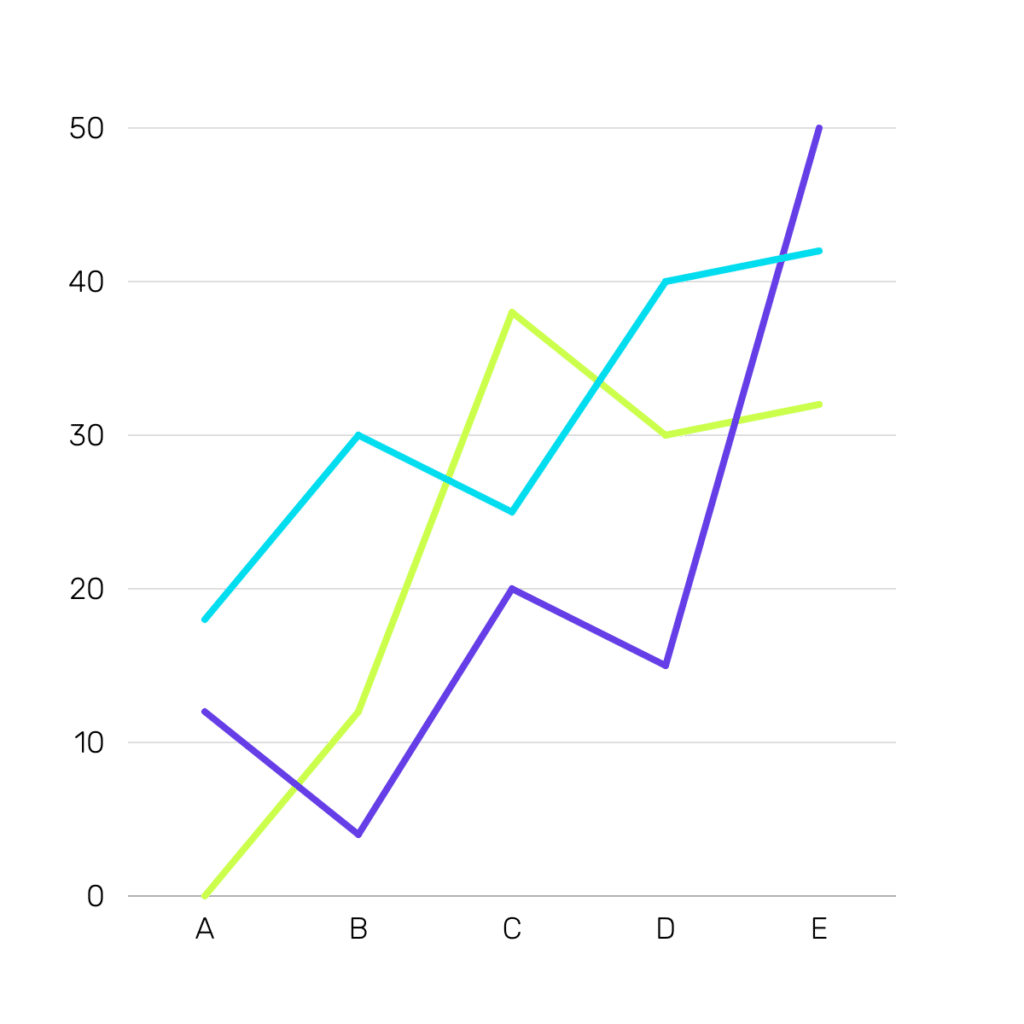
With the suggestions we received from Veda, we determined which changes we could automate and which ones may need further information from the provider. This drove multiple processes for us to build or modify to accommodate. Then we started to integrate the changes into our systems and review the results of the next month’s audit. This is one barometer of how the changes are affecting our accuracy. We continue to look for opportunities in the data and Veda helps us to focus on areas that may get the biggest return. We work together to see what is most feasible, as this is a partnership that includes our providers who want to get on board to help us on the journey. This process improves the experience for the providers’ patients and Medica’s members.
How do you report your department’s work and results within the organization?
We have a dashboard that goes to senior leadership that reports our accuracy rate and compliance. Of course, it’s always exciting to see accuracy increasing and bad data consistently being corrected. Our reporting helps highlight both gaps and opportunities.
How have you seen data accuracy positively impact member experience?
Accuracy, adequacy, and efficiency are what our members expect and we want to deliver. They depend on us for their healthcare needs and it starts with knowing they can view our directories to find a provider near them to take care of their family’s health. As we all know, health care is complicated, so it is our job to make things easier in whatever ways we can. My role is to focus on ensuring that the data we receive is accurately displayed to our members and they can trust it.
As Director of Provider Operations and Initiatives, Patty is responsible for Medica’s provider network data in online and print directories. Based in Minnesota and with Medica for over 18 years, Patty oversees network compliance and adequacy. Connect with Patty on LinkedIn.


