By Meghan Gaffney
Here’s something you’ve heard before—patients are now becoming “consumers” of medical care in the same way that they make informed choices in retail and other aspects of their lives. From the patients’ point of view, the healthcare system is broken, with significant issues arising around cost, access, and quality of care.
Link to Healthcare Business Today article
The patients aren’t wrong. Over one trillion dollars is spent each year on healthcare administration alone. Those providing and subsidizing healthcare are equally frustrated by the inefficiencies and challenges that exist on the administrative front.
Value-based care (VBC) and reimbursement models have long been hailed as the solution to these problems. However, anyone who works in healthcare knows that adoption of true risk-based models has been slow. Let’s explore why. We can start by exploring the history of VBC, shed light on the “missing ingredients” for making VBC a success, and then dive into how data–specifically advanced processing of data through automation–is the key to breeding trust and accelerating the shift away from fee-for-service.
What has prevented VBC models from becoming the norm? The missing ingredient
The first VBC pilots were rolled out by Medicare well over a decade ago, yet here we are, still operating in a predominantly fee-for-service system, rather than on the other side of the transition to value as anticipated. Oftentimes, the logistics of bringing together different stakeholders and disparate systems are pinpointed as the root cause of the issue. And it’s true, to say that the logistics are complicated is an understatement at best.
But I would argue that the logistics don’t present insurmountable obstacles.What was lacking was the key ingredient to all lasting and transformative relationships– trust. For value-based contracts to operate as intended, providers and payers must have a certain level of trust in each other, as well as in the data that connects their systems and informs their mutual decision-making. The foundation of trust in financial arrangements is always data, and healthcare’s limited technological advances have prevented not only data-sharing between parties in VBC agreements, but “good” data-sharing. The result is an inability to trust that either side has the quality of data required to accurately assess cost and performance.
The role technology can play in deepening trust by improving data quality
That’s the “bad news.” But I’m delighted to say that there’s actually quite a bit of good news. While healthcare has long been a laggard when it comes to technology adoption, the pandemic spurred accelerated adoption of AI and automation and played a critical role in moving the industry forward. The tech is ready—and now the stakeholders who truly need the tech are ready to use it.
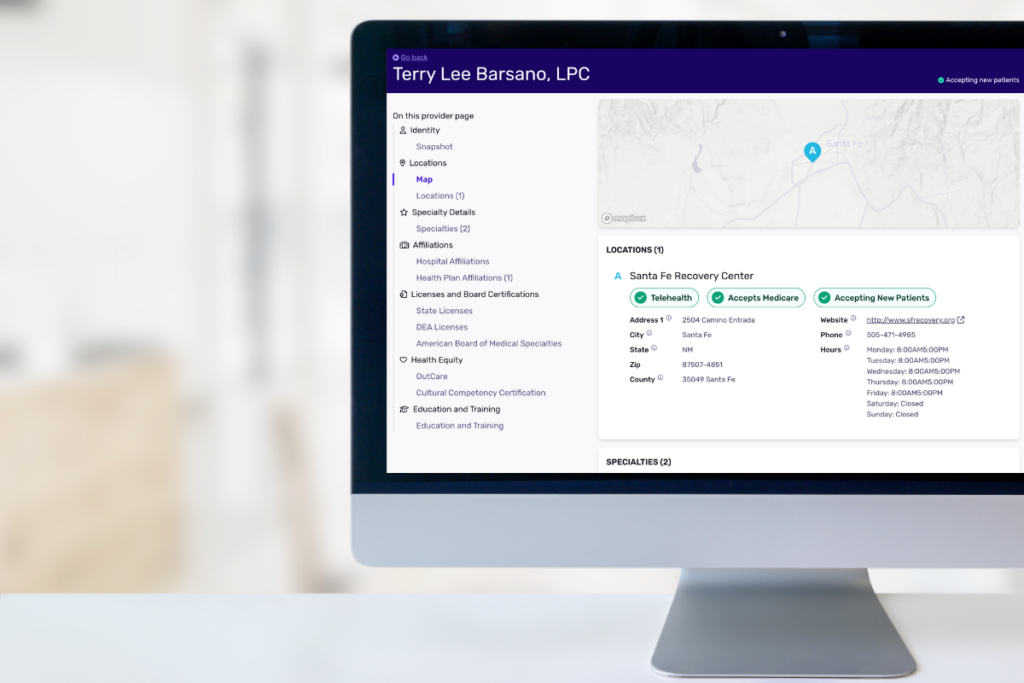
With this in mind, let’s look at a use case that illustrates the need for technology that improves data accuracy and transparency and therefore promotes trust, the missing ingredient in VBC. In order to get their members the care they need, payers (i.e., insurance companies) have to be in constant contact with provider organizations. Provider organizations often send data updates on participating providers infrequently and equally often those files have errors. The data are also manually keyed in by associates at the payor, a process that takes weeks and tends to create duplicative or incomplete records, as well as further contributing to inaccuracy.
This exact issue derailed a VBC pilot program that my business was a part of. A state-based health plan we worked with backed out of their VBC agreement due to lack of provider data transparency. Each month the payor attempted to reconcile which claims could be attributed to VBC contracts. There were discrepancies in the participating provider rosters that slowed this process down, and eventually, ground the entire project to a halt. Data is core to establishing trust in these agreements, and illustrates how hard it is to execute them as designed in the face of poor-quality data. And remember, this is just a single use case. There are many more.
Ensuring that the tech being used is as transparent as it is efficient
That annual trillion dollars in administrative spend in healthcare is a major issue negatively impacting all parties involved. In a VBC or any kind of contract, the goal should always be to provide patients with the best care possible while decreasing costs. Right now, a huge driver of administrative spend is the cost of manually processing data and the downstream waste that happens when data is inaccurate. A huge step forward is ensuring there’s data transparency so that inaccuracies can be identified and addressed.
So, what does transparency look like from a technology standpoint? What should payers be looking for when shopping for solutions to automate their data? Provider groups and their payor partners need a solid foundation of data to measure performance for VBC agreements, and they also need to understand how these measurements are made. Vendors that offer data solutions should always be ready to walk their clients through their processes and make clear how accurate data is obtained, maintained, and measured. Some technology vendors even build accuracy guarantees right into their contracts.
This level of transparency in vendor-payer relationships eliminates any potential mistrust in the tech itself, which has been a driving factor in AI’s relationship to VBC. In the event something does go wrong, there is a pre-established measurement system that both parties understand and that can be used to easily identify where the error occurred.
Is AI the solution to accomplishing our VBC goals faster?
I think so, yes, but with an important caveat–the AI vendors need to build trust, too. I’ve seen first-hand within my company and from industry peers the power that data automation tech solutions have when they’re a part of contracts built on trust in the tech and the people behind it. Understanding that trust is the missing ingredient with provider-payer relationships—and by extension, other key relationships such as those with technology vendors—is key to making inroads with future partnerships.
The pandemic spurred increased health tech adoption at the same time that patients were paying much more attention to their health and engaging with medical services as savvy consumers. These factors have moved the industry to a point where it is truly ready to accelerate VBC.