Resources > Press
Introducing Velocity: A Solution to Help Health Plans Comply With the No Surprises Act
Introducing Velocity: A Solution to Help Health Plans Comply With the No Surprises Act
With the No Surprises Act, as part of the Consolidated Appropriations Act, going into effect on January 1, 2022, stakeholders across the healthcare system are working hard to get their organizations into compliance with the various provisions of the new law.
NO SURPRISES ACT AND ITS IMPACT ON PROVIDER DIRECTORIES
Much of the attention on the No Surprises Act has been around the protection it offers consumers from unexpected medical bills arising from circumstances beyond their control. To help achieve the goal of eliminating surprise billing, the No Surprises Act contains a provision that requires health plans to make updates to their provider directories within 48 hours. Updated, accurate directories make it easier for members to determine if a doctor is in-network. With just a few weeks until the law goes into effect, health plans need to be laser-focused on their ability to meet this requirement.
But a lot goes into keeping those directories updated. The traditional manual data entry method is fraught with issues: provider updates currently take weeks and often only yield 60-70% accuracy rates. And by the time the process is done, the data is outdated. No matter how many extra hands are available to put on keyboards and enter this data, due to the sheer volume it is virtually impossible to significantly reduce processing time with such a manual approach. And the probability of introducing errors into the data would only increase with additional human touchpoints.
INTRODUCING VELOCITY: DIRECTORY UPDATES PROCESSED IN LESS THAN 24 HOURS
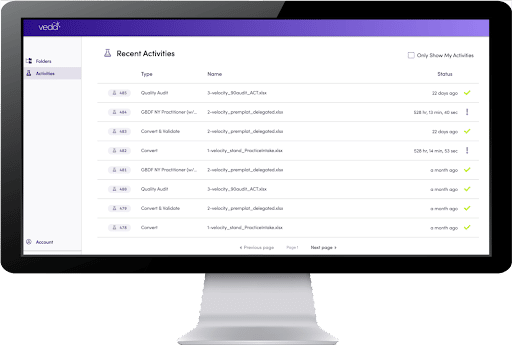
Our platform allows you to process—format, validate, and correct—provider data files and update the data in your system in less than 24 hours. Guaranteed. All while saving costs and improving accuracy. By automating roster intake, we reduce human processing and reduce human error.
Trusted by six of the top 10 U.S. health plans, veda Velocity uses AI and machine learning to help plans transform and enhance their provider data—achieving fast, accurate, and No Surprises Act-compliant results that otherwise would not be possible.
The platform takes unstructured roster files from provider organizations and standardizes them into the health plan’s preferred format. The smart automation solution improves productivity by 10-12x and reduces data processing time by 98%, allowing plans to publish directory updates in 24 hours or less. Files are verified, corrected, and updated—all within the plan’s existing database.
VEDA VELOCITY PLATFORM FEATURES
It’s truly as easy as drag and drop, run, and download. We offer the fastest workflow, the highest accuracy, and the greatest ROI for processing provider data.
- Intake
Automating the manual workflow. Roster files are read, identified, and formatted for use in a health plan’s downstream systems. With our machine learning tool, the more you use the application, the more concepts it will recognize.
- Validate
Stopping bad data from entering your system. Data is validated against external source(s)to verify if the existing information is current or requires updating. Our platform sources NPPES, CMS, DEA, and state licensing organization data to verify if your existing information is correct or needs updating.
- Enhance
Simplify audits with cleaner data. Through our external validation sources, we provide an audit on data intake. You’ll receive a file report for updating missing or incorrect information in your internal database(s).
- Compare
Integrating to quickly update your database. Automatically compare the incoming rosters to your downstream systems: identifying what provider data is new, what needs to be changed, and what needs to be removed. We can custom integrate or set up an SFTP based on your plan’s preference.
REAL-WORLD RESULTS
Our customers are seeing real-world results every day. While we guarantee 24-hour turnaround and delivery within the MSA, many see results even faster. One existing customer—a top 10 national payer—sees 99% of rosters processed and delivered in under four hours.
Another national health plan had our data accuracy verified by a third-party audit and confirmed that our data is more than 99.5% accurate compared to external sources such as CMS, DEA, NPPES, and State licensing organizations.
Our platform allows you to process provider data files in less than 24 hours. Guaranteed. All while saving costs and improving accuracy.
SCHEDULE A DEMO
Shifting directory updates from six weeks down to a few hours may sound impossible, but with veda it’s simple. To see Velocity in action, schedule a demo today.
THE TOP CHOICE FOR HEALTH CARE
We're the authority on health plan data. See how Veda's Smart Automation platform can work for your health plan. Improve data accuracy, reduce workloads, and enhance the member experience. But first, start with a free demo.